[ad_1]
As a child, Dr. Alika Lafontaine had a stutter and was labelled as having a learning disability. He says teachers told him he would never graduate high school.
“I definitely had learning challenges,” Lafontaine told White Coat, Black Art‘s Dr. Brian Goldman. “People were quick, I think, as a kid, to label me as somebody who just couldn’t achieve because of this.”
On Aug. 21, Lafontaine takes over as president of the Canadian Medical Association (CMA), becoming its first Indigenous leader.
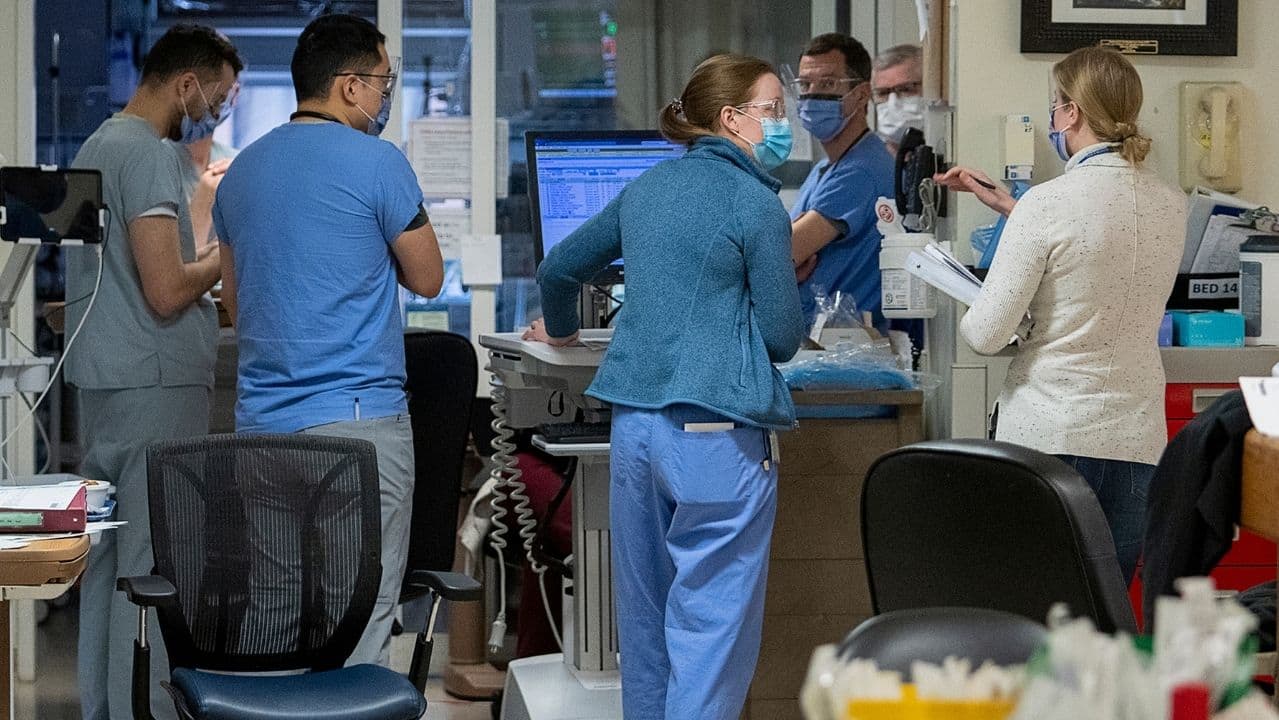
It comes at a time when the health-care system is reeling from challenges exacerbated by the pandemic: doctors suffering burnout, nurses quitting in droves and patients facing lengthy ER wait times.
As CMA president, he’ll oversee more than 68,000 member physicians and trainees. The organization is the largest advocacy group for medical doctors in Canada.
“Leadership is a continuum where you think at the beginning the most important part is having the loudest voice, and at the end, you’ve realized the most important part is amplifying other people’s voices,” said Lafontaine.
“I hope that physicians across the country feel like they’re heard in ways that they haven’t been heard before.”

Born and raised in Treaty 4 territory in southern Saskatchewan, Lafontaine works as an anesthesiologist at Grande Prairie Regional Hospital in Alberta.
He says the personal challenges he faced growing up, and his experiences as an Indigenous doctor — he has Métis, Ojibway, Cree and Pacific Islander ancestry — help in understanding those who have felt that they have no voice.
With his parents’ support and belief that education was “the pathway to a better life” — and that their son could become something more than teachers expected of him as a child — Lafontaine’s mother pulled him out of grade school and home-schooled him.
Childhood experiences a ‘huge motivator’
By age 14, Lafontaine says he graduated high school. He went on to medical school and finished his residency by the time he was 28.
“That kid that was labelled with a learning disability — you know, at one time, I had no voice. At one time, people looked at me as broken,” said Lafontaine, who also grappled with hearing issues caused by ear infections when he was younger.
Lafontaine described those childhood experiences as a “huge motivator” for him.
He spoke with Goldman about his hopes and priorities as CMA president. Here is part of their conversation.
Not a day goes by without hearing on social media about an emergency department that’s closing for a few hours or a few days. What’s your take on what’s going on? Because there are people who are saying the system’s close to collapse, which I think is probably an exaggeration.
I think it depends on kind of the place that you’re at. Health human resource crises hit people differently depending on the availability and options for services.
If you have one emergency room for the entire city, like here in Grand Prairie, health human resource crises are going to hit us a lot differently.

Has [the Grande Prairie] emergency department ever closed?
This one hasn’t. But there’s a lot of emergency departments in the surrounding area that have closed, and that’s put a lot more pressure on our [ER] obviously, because patients need to be seen somewhere for the problems that they have.
I do think in certain areas, things are on the brink of collapse. I think those places tend to be outside of our major centres.
I think the stresses of having to be on all the time is something that health-care workers across the spectrum normalized. It became a very normal thing for nurses to be denied vacation, to be mandated to come back into the hospital. It became a very normal thing for physicians to work far beyond their exhaustion, tolerance.
We’re now living in this environment where we have this backlog of care … hundreds of thousands of people that didn’t get care because we shut down care mid-pandemic because of what happened with just overloading our hospitals and other things.

People now have enough space to realize the things that we did during COVID aren’t normal things for us to do, and there’s repercussions to everything that we do, right?
The … consequence of never taking time off work is you damage your body, you damage your relationships, you damage your ability to be happy and hopeful. People need space to recover. And sometimes that space is just not given because the system has become used to just saying, “Get on with it. You need to come to work.” And as a result, people are walking away.
You’re about to assume the mantle of president of the Canadian Medical Association. How does that feel?
It is surreal. I reflect on the confidence that my colleagues in Alberta put in me by choosing me as the next CMA president, and also … the mantle of being the voice of Canadian physicians and kind of what that means.
The role of the CMA president is to help people understand how their day-to-day work fits within the broader context of the health-care system. You know, how do you tie in the aspirational goals that you have for care when they come into contact with the resistance from the system to do things better?
Canada’s stumbling health-care system is now facing funding and staffing challenges that threaten the entire sector. Burnt-out and over-worked nurses are quitting in droves, while jurisdictions struggle to convince them to stay. Health-care workers share the changes they say would help them keep going.
I think to a great degree, physicians across the country are really suffering from feeling like … they’re not as important in the lives of their patients anymore … sometimes they feel like they’re suffering alone when we’re all kind of suffering together.
And the opportunity for myself in the role of CMA president … is to be someone who can kind of draw those pieces together again.
Healing is going to take a long time. It obviously won’t be 100 per cent solved within the year that I’m president. But I think we can all make a major impact when we speak truth in the places that we stand.
You’re the first Indigenous physician in this role. What do you want to accomplish as Canada’s first Indigenous CMA president?
I would really like to normalize that Indigenous physicians can fill these positions — can lead these organizations.
It’s a part of just creating space for not just Indigenous communities, but communities that haven’t been at the table who should be at the table.
Dr. Alika Lafontaine discusses possible solutions to improve health care in Indigenous communities and his award from the Public Policy Forum.
I think we all know logically that we’re trying to solve problems, [and] if we don’t bring the people who are actually suffering from the problems to the table, we miss out on the most important parts of understanding the problem and within systems that have historically excluded voices or, you know, pushed people away from the table.
I think that’s the power of having voices in positions — people in positions who’ve never filled them before — is they can see who’s missing.
Written by Ruby Buiza. Produced by Jeff Goodes and Dr. Brian Goldman with help from Amina Zafar. Q&A edited for length and clarity.
[ad_2]
Source link